of approximately 55 kb isolated from MDR S. typhi
having ACCoT-resistance (Fig. 3).
Figure 3: Agarose gel electrophoresis of plasmid
DNAs
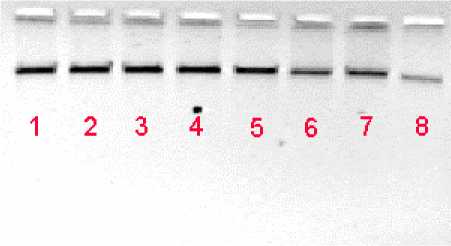
Lane 1: S. typhi strain BS13 (ACCoT) of 1991; Lane 2: E. coli
strain EC3 (NxCpACCoT); Lane 3: S. typhi B72
transconjugant (pEC3); Lane 4: K. pneumoniae strain K1
(ACCoT), Lane 5: S. typhi B72 transconjugant (pK1); Lane 6:
P. vulgaris Prv2 (ACCoT)); Lane 7: S. typhi B72
transconjugant (pPrv2); Lane 8: plasmid size marker of 53.7
kb from E. coli V517.
Discussion
S. typhi is noteworthy in the etiology of outbreaks and
sporadic cases of typhoid fever, an endemic disease in
India. Presently, enteric fever caused by MDR S typhi
continues to be a problem across the country. Such
multidrug resistance in S typhi has been reported to be
plasmid mediated.(2-10) The plasmid mediated en
bloc transfer of ACCoT-resistance of S. typhi isolates
has been reported earlier from different parts of
India.(19, 20) Karmakar et al. (11) reported 120 kb
plasmid encoding resistance to A, C, T, and
streptomycin (S) in S. typhi isolates from Kolkata
during 1989-1990 enteric fever epidemic. Haldar et al.
(21) reported a transferable plasmid carrying
resistance genes for A, C, T and S in S. typhi isolates
from Kolkata in the year 1995. Many other authors
(5,9,10) from different parts of the world reported the
plasmid-mediated resistance of A, C, Co and T in S.
typhi isolates and that these plasmids are large
(approximately 180 kb) and conjugative, and
originated from Southeast Asia.
In the present study, results of the primary and
secondary conjugation experiments revealed that
resistance to A, C, Co and T of S. typhi isolates
associated with enteric fever outbreaks in three
different regions of West Bengal in 1991 was
transferable. When S. typhi isolates, obtained in the
years 1992 and 2000, having the common resistance
pattern (ACCoT) were investigated, these also
showed transferability of ACCoT-resistance. The
transconjugants were selected using C, but on
antibiotic susceptibility testing we found the
transconjugants exhibiting resistance to A, Co, T, in
addition to C, with MICs similar to that of their
corresponding donor strains (Table 1). This finding
prompted us for an investigation of R-plasmid
contained in them. Agarose gel electrophoretic
analysis revealed the presence of a single plasmid of
approximately 55 kb among the isolates associated
with the 1991 enteric fever outbreak. The
corresponding transconjugants also contained the
similar plasmid. The same plasmid patterns of MDR
isolates from three outbreak regions suggest the wide
spread occurrence of plasmid mediating ACCoT-
resistance of outbreak causing S. typhi in different
parts of the state West Bengal in 1991. MDR S. typhi
with similar antibiogram, which had been isolated in
different years (1992 and 2000) of the present study,
contained the same plasmid. This phenomenon
indicated the existence of a plasmid carrying ACCoT-
resistance in the bacterial population in this region.
In our studies, there was co-existence of antibiotic-
sensitive and MDR strains of S. typhi (22), but unlike
MDR strains the sensitive strains did not contain any
plasmid. The presence of conjugative R-plasmid in
MDR S. typhi and absence of any plasmid in the
sensitive strain has been reported earlier by
researchers from Kolkata, India.(11) R-factors
originally found in community isolated E. coli strains,
in Mexico, transferred by in vitro conjugation
experiments to S. typhi, in which the R-factor found
unstable after 100 generations in liquid culture.(23)
Thus, in S. typhi the R-plasmid is an unstable plasmid
that may appear or disappear at any time resulting in
the emergence of drug resistant or drug sensitive
isolates. The selection exerted by antibiotic treatment
of enteric fever may be the cause of acquisition of R-
plasmid.(24) Through the acquisition of a plasmid
conferring multidrug resistance, the strain undergoes
the necessary and appropriate adaptation for survival
in the changing antibiotic environment. Thus, it
appears that the already existing sensitive strain, by
the acquisition of a R-plasmid, has emerged as a
resistant strain within the S. typhi bacterial population
in and around Kolkata, and has been able to adapt the
challenge of antibiotics as they are introduced into
clinical medicine. But what might be the reservoir
host of the R-plasmid from which the sensitive S.
typhi strain could acquire it (R-plasmid) during
adverse situation?
The prevalence of S. typhi harbouring the plasmid
encoding ACCoT-resistance in Kolkata has not yet
been studied. We suspected that the resistance
plasmid might have been transferred from other
More intriguing information
1. Running head: CHILDREN'S ATTRIBUTIONS OF BELIEFS2. The name is absent
3. Willingness-to-Pay for Energy Conservation and Free-Ridership on Subsidization – Evidence from Germany
4. Auction Design without Commitment
5. The Challenge of Urban Regeneration in Deprived European Neighbourhoods - a Partnership Approach
6. The name is absent
7. Uncertain Productivity Growth and the Choice between FDI and Export
8. Modeling industrial location decisions in U.S. counties
9. Estimating the Technology of Cognitive and Noncognitive Skill Formation
10. The name is absent