Purerfellner H., Aichinger J., Martinek M., Nesser H.J., Janssen J, 15
“Short- and long-term experience in pulmonary vein segmental ostial ablation for
paroxysmal atrial fibrillation”
Moreover, interesting and promising efforts are made by one manufacturer (Stereotaxis,
Inc) to conduct an ablation procedure by remote navigation of the ablation catheter which is
directed by a strong magnetic field around the patient´s body.
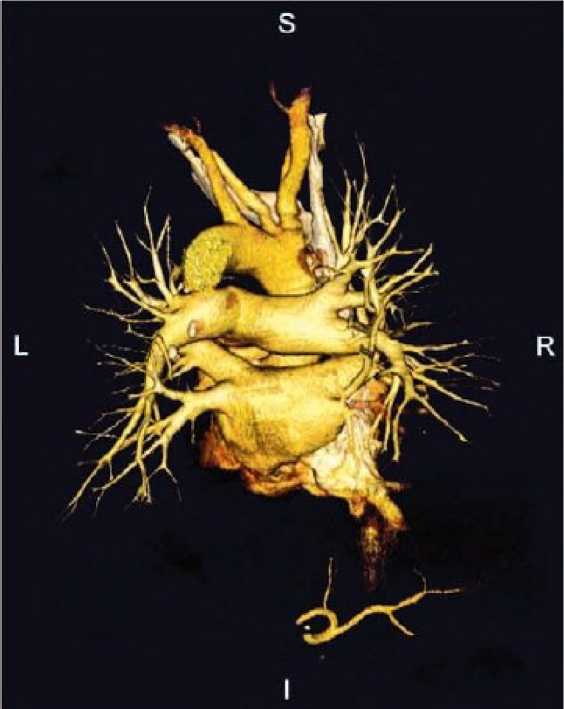
Figure 6: Multislice CT demonstrating aortic (above), pulmonary arterial (mid) and pulmonary
venous vasculature (posterioanterior projection)
Conclusion
The CRR in patients with medically refractory PAF undergoing ostial PVI accounts for
78% after a short term follow up of 6 months. A 4 PV procedure (including the RIPV) warrants
a higher CS. In patients with a 3 PV procedure (sparing the RIPV) the CRR in the longterm
follow up is reduced to 62%. However, the CS rate seems to be constant, whereas the PS is
reduced. PV stenosis is the main cause for complications. In addition to an exact analysis of
procedural parameters a longer follow up period seems necessary to better quantify the clinical
benefit to risk ratio of segmental ostial PVI in contrast to other strategies in the treatment of
atrial fibrillation.
References
1. Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic
beats originating in the pulmonaty veins. N Engl J Med 1998;339:659-666.
2. Haissaguerre M, Shah DC, Jais P et al. Electrophysiological breakthroughs from the left
atrium to the pulmonary veins. Circulation 2000;102:2463-2465.
Indian Pacing and Electrophysiology Journal (ISSN 0972-6292), 6(1): 6-16 (2006)
More intriguing information
1. KNOWLEDGE EVOLUTION2. Trade Liberalization, Firm Performance and Labour Market Outcomes in the Developing World: What Can We Learn from Micro-LevelData?
3. Quelles politiques de développement durable au Mali et à Madagascar ?
4. The name is absent
5. Response speeds of direct and securitized real estate to shocks in the fundamentals
6. PROTECTING CONTRACT GROWERS OF BROILER CHICKEN INDUSTRY
7. The name is absent
8. Feature type effects in semantic memory: An event related potentials study
9. Handling the measurement error problem by means of panel data: Moment methods applied on firm data
10. Opciones de política económica en el Perú 2011-2015